- This Discussion Thread has 14 replies, 10 voices, and was last updated 1 week, 4 days ago by Adetola.
-
AuthorPosts
-
-
2024-04-15 at 11:52 pm #12398GraceKeymaster
Thinking of your current or a past practice area provide an example of the train of transmission specific to that area. Fill in all ‘links’ in the chain with an example for each link:
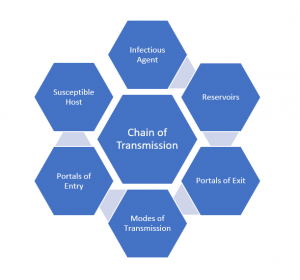
Infectious Agent:
Reservoirs:
Portals of Exit:
Modes of Transmission:
Portals of Entry:
Susceptible Host:
-
2026-01-19 at 8:58 pm #18285MildredMember
Chain of Transmission – Medical–Surgical Unit
Infectious Agent:
Clostridioides difficile (C. difficile)Reservoirs:
Gastrointestinal tract of infected or colonized patients
Contaminated surfaces (bed rails, call bells, toilets, commodes)
Contaminated healthcare workers’ hands
Portals of Exit:
Feces from an infected or colonized patient (during bowel movements or incontinence episodes)
Modes of Transmission:
Indirect contact transmission via the contaminated hands of healthcare workers
Contact with contaminated equipment or environmental surfaces (e.g., shared commodes, improperly cleaned rooms)
-
2026-01-23 at 3:59 am #18318ArleneMember
Hi Mildred
C-Diff must be one of my most feared infections as it is so difficult to remove/treat increasing the chance of transmission.
Lack of education – Not all health care providers are aware that alcohol-based hand rub (ABHR) is not an effective way to remove C-Diff from hands therefore soap and water must be used.
Accessible facilities – Many times, the inconvenient placement of sinks within facilities prevent the accessibility of soap and water hand washing as frequently as needed.
Your document seems to have cut off “Portals of Entry” (fecal-oral) and “Susceptible Host” (immunocompromised, previous antibiotic use).
-
-
2026-01-20 at 12:27 pm #18292Carla-JaneMember
Chain of Transmission; Long Term Care Facility
Infectious Agent : Norovirus
Reservoirs: Infected residents, Contaminated surfaces, Contaminated food or water
Portals of exit: Vomit, Feces, Respiratory droplets. The virus exits the body primarily through gastrointestinal secretions.
Mode of Transmission: Direct contact – hands of healthcare workers or residents after toileting.
Indirect contact – touching contaminated surfaces or shared equipment.
Fecal-oral transmission – Ingestion of virus particles due to poor hand hygienePortal of Entry: Mucous membranes (mouth or nose), Ingestion of contaminated food or hands
Susceptible Host: Older adults with weakened immune systems, residents with chronic illness
-
2026-01-24 at 4:59 pm #18330JasvirMember
I like your example because norovirus is really common in long-term care and spreads very fast. It shows how even small things, like missing hand hygiene after toileting residents or touching shared equipment, can quickly affect many residents. The part about older adults being more vulnerable also stood out to me. It’s a good reminder of why infection control is so vital in LTC, not just for policy, but for real people’s safety.
-
2026-01-28 at 5:58 pm #18371MujidatMember
This is a very clear and well-organized example of the chain of transmission, and norovirus is especially relevant in long-term care settings. You accurately identified infected residents and contaminated surfaces as key reservoirs, which reflects how easily norovirus can persist and spread in shared environments.
I also like how you clearly explained the fecal-oral route and connected it to poor hand hygiene after toileting, as this is one of the most common ways norovirus outbreaks occur in LTC facilities. Your inclusion of both direct and indirect contact highlights the importance of environmental cleaning and proper hand hygiene for staff and residents
-
-
2026-01-23 at 1:04 am #18313ArleneMember
Chain of Transmission – Psychiatric ICU
Infectious Agent: MRSA
Reservoirs-
High touch surfaces (shared bathrooms, door handles), Nasal passages, medical equipment, linens, skin of infected or colonized individuals, contaminated hands of healthcare workers.Portals of Exit-
Respiratory secretions, wound drainage, Skin of colonized or infected individualsModes of Transmission-
Direct: Healthcare workers hands; contact with skin or respiratory secretions of an infected or colonized individual;
Indirect: Medical equipment (Vitals machines); door handles; linens; healthcare workers clothingPortal of Entry –
Break in skin (open wounds), invasive devices (Peripheral/central lines), mucous membranes (nasal passages, mouth)Susceptible Host-
Immunocompromised individuals; Patients with invasive medical devices; open wounds -
2026-01-24 at 2:54 pm #18326Aleena MaryMember
Chain Of Transmission- MRSA in Hospital .
Infectious Agent: MRSA Bacteria.
Reservoirs: Patients who are colonized or infected, Healthcare workers’ hands or clothing,Contaminated medical equipment (bed rails, IV pumps).
Portals of Exit: Open wounds or surgical sites,Respiratory secretions, Skin flakes.
Modes of Transmission: Direct contact: touching the infected patient
Indirect contact: touching contaminated surfaces or instrumentsPortals of Entry: Breaks in the skin, mucous membranes.
Susceptible Host: Patients with weakened immunity, Elderly, infants, or those recovering from surgery, Anyone with chronic illnesses or open wounds
-
2026-01-24 at 4:51 pm #18329JasvirMember
Chain of Transmission -Community Care
Simple things like hand hygiene, cleaning equipment, and using PPE properly really matter because, in my experience, respiratory infections such as the flu or COVID-19 are common in home care. Here is an example of the chain of transmission in this setting:
Infectious Agent: Influenza or COVID 19 virus
Reservoirs: Client or family members in the home
Portals of Exit: Coughing, sneezing, talking
Modes of Transmission: Droplets, hands, shared surfaces/equipment
Portals of Entry: Nose, mouth, eyes
Susceptible Host: Older adults, clients with chronic illness or immunocompromised, and caregivers -
2026-01-28 at 5:34 pm #18370MujidatMember
Practice Area: Long-Term Care Facility
Infectious Agent:
Respiratory Syncytial Virus (RSV)Reservoirs:
Infected residents, staff, or visitors carrying RSV; contaminated surfaces such as bed rails, call bells, wheelchairs, and shared equipmentPortals of Exit:
Respiratory secretions are released through coughing, sneezing, talking, or nasal drainage
Modes of Transmission:Direct contact with infected respiratory secretions
Droplet transmission during close contact
Indirect contact via contaminated hands, clothing, or environmental surfacesPortals of Entry:
Mucous membranes of the nose, mouth, or eyesSusceptible Host:
Older adults, residents with chronic lung or heart disease, immunocompromised individuals, and those living in close-contact environments-
2026-01-29 at 9:26 pm #18384MeboMember
Hello Mujidat
Thank you for sharing RSV in Long term Care, and I agree is huge significant concern in Long term care setting from experiencing
working in LTC for over 5 years, and from infection- control perspective, rapid implementation of Droplet and conta precautions is
very essential once an outbreak is declared. Most Importantly hand hygiene remain one of the most effective intervention, environment
cleaning espeacially high touch areas.
-
-
2026-01-29 at 9:14 pm #18383MeboMember
Hospital Acute Care- CPO (Carbapenemase- producing Organisms
Infectious Agent: Escherichia coli, Enterobacter spp
Reservoirs: colonized or infected patients – GI tract, wounds, respiratory tract
Portals of Exit: feces (most common), wound drainage, urine
Modes of Transmission: direct or indirect contact- health care workers hands touching infected patients body fluids, shared patient rooms or bathrooms
Portals of Entry: Hands touching mucous membranes (eyes, nose, mouth)
Susceptible Host: Elderly or immunocompromised patients, ICU patients, Patients on broad – spectrum antibiotics -
2026-02-09 at 12:39 pm #18481JamesMember
Chain of transmission: Long-term Care
Infectious Agent: Covid-19
Reservoirs:
Human respiratory tract, contaminated surfaces, health care workers
Portals of Exit:
Respiratory secretions from the nose and mouth whether it be from coughing, sneezing or talking.
Modes of Transmission:
Respiratory droplets
Indirect contact via contaminated surfaces
Portals of Entry:
Mucous membranes of the eyes, nose and mouth, respiratory tract
Susceptible Hosts:
Individuals not naturally immune to the virus, the elderly, people with autoimmune disorders and chronic illnesses, as well as people who haven’t been vaccinated.-
2026-02-09 at 1:31 pm #18482AdetolaMember
Great example of the chain of transmission in a long-term care setting. You clearly identified COVID-19 as the infectious agent and accurately linked the human respiratory tract and contaminated surfaces as key reservoirs. I also like how you highlighted multiple portals of exit and entry, which reflects how easily COVID-19 can spread in shared living environments. Identifying elderly residents and those with chronic or autoimmune conditions as susceptible hosts is especially relevant in long-term care, where residents are at higher risk for severe illness. Overall, your examples clearly show why strict infection-prevention measures are essential in this setting.
-
-
2026-02-09 at 1:34 pm #18483AdetolaMember
Chain of Transmission – Long-Term Care (C. difficile)
Infectious Agent:
Clostridioides difficileReservoirs:
Infected or colonized residents; contaminated surfaces such as toilets, bed rails, commodes, and shared equipmentPortals of Exit:
Feces from residents experiencing diarrheaModes of Transmission:
Indirect contact through contaminated hands of staff or contaminated surfaces and equipmentPortals of Entry:
Mouth (ingestion of spores via hands or objects)Susceptible Hosts:
Older adults in long-term care, residents on antibiotics, and those with weakened immune systems
-
-
AuthorPosts
- You must be logged in to reply to this Discussion Thread.