- This Discussion Thread has 11 replies, 8 voices, and was last updated 3 weeks, 2 days ago by Mebo.
-
AuthorPosts
-
-
2024-04-15 at 11:52 pm #12397GraceKeymaster
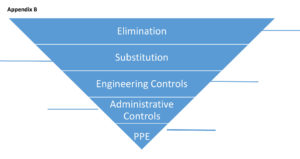
Reflection activity: Thinking of your current or a past workplace provide specific examples of each hierarchy of control – see Appendix B.
-
2026-01-22 at 10:29 pm #18310Carla-JaneMember
Elimination: removal of fabric furniture that cannot be properly disinfected especially after an outbreak.
Substitution: replacing harsh cleaning chemicals with hospital grade disinfectant that are safer for residents with respiratory issues (COPD, Asthma).
Engineering control: installing hands-free sinks and hand sanitizers at every room entrance. bed and door alarms for residents at risk of elopement.
Administrative Controls: enforcing policies for hand hygiene, outbreak management, enhancing cleaning schedules for high-touch surfaces like railings, door knobs.
PPE: gloves and gowns for residents on contact precautions, N95 respirators for airborne risks, Masks and eye protection during respiratory outbreaks (COVID-19, influenza).-
2026-01-23 at 4:08 am #18319ArleneMember
Hi Carla-Jane
You prevention strategies are insightful. I noticed more replacement of fabric surfaces within healthcare settings post-covid. Our hospital is replacing curtains with a “antimicrobial fabric”. I always shake my head when I see a “partial” implementation of practices. An example is a public bathroom that has touchless soap dispensers, but manual water faucets and air hand dryers. I have read some studies that show some evidence that the hand dryers actually spread microbes into the air. Sometimes it is difficult to not touch the dryer, leaving me to question “how many other people touched the dryer without using soap when washing their hands?”
-
-
2026-01-23 at 2:25 am #18314ArleneMember
Elimination: Proper and adherence to hygiene, cleaning high touch areas, access to appropriate cleaning supplies, removal of hazardous objects from persons and patient-care areas (weapons, pencils, strings (ie: hoodie, shoes).
Substitution: Unscented cleaning chemicals over harsh products (respiratory and migraine health risks); Skin-friendly hand sanitizer (reduce R/F skin breakdown), markers provided to patients rather than pencils
Engineering control: Plexiglass in patient rooms and nursing station, ventilation systems and HEPA filters, POC sharps containers, POC hand sanitizer pumps, safety needles.
Administrative Controls: Active and passive screening, self reporting, symptom surveillance, IPAC policy and implementation (enforced by audit results ie: hand hygiene and CAUTI); outbreak management and prevention (Admission ARO testing); Implementation of EIPAC Framework to guide and improve adherence to IPAC policies, Safe nurse-patient ratios, staff training (IPAC, SMG, WHMIS, job-specific training)
PPE: Access to PPE equipment, proper selection and use of PPE (N95 fit testing; adequate training); Proper maintenance of PPE (not expired, inspected, proper storage), POC Risk assessments.
-
2026-01-26 at 3:55 pm #18357JasvirMember
I like how detailed your examples are, especially for administrative controls. It really shows how much planning and policy go on behind the scenes to keep everyone safe. I also liked your substitution examples with unscented cleaners and skin-friendly sanitizer. That’s something people don’t always think about, but it really matters for staff and patients in the long term.
Your post made me realize how all the levels work together, not just PPE. It’s a good reminder that safety starts long before we even put on gloves or a mask.
-
-
2026-01-26 at 3:48 pm #18356JasvirMember
From my experience in home/community care, here are some examples:
Elimination: Screening clients for symptoms before visits and postponing non-urgent visits when someone is sick.Substitution: Using virtual/phone check-ins instead of in-person visits when possible.
Engineering controls: Use hand sanitizer stations, properly labelled sharps containers, and maintain good ventilation by opening windows during visits (depending on the weather).
Administrative controls: Following agency policies, IPAC training, visit scheduling to limit exposure, and clear cleaning protocols.
PPE: Wearing gloves, masks, and eye protection for direct care or if a client has respiratory symptoms.
Module 2 reminded me that PPE is very important, but it should be the last line of defence. Using the higher levels first helps reduce risk for both clients and us healthcare workers.
-
2026-01-28 at 6:09 pm #18373MujidatMember
Thank you for sharing your examples—they clearly illustrate how the hierarchy of controls can be applied in home and community care. I like how you emphasized screening and postponing visits as elimination, which is such a proactive step in preventing illness before it even enters the home. Your examples of substitution with virtual visits and engineering controls like hand sanitizer stations and ventilation show how practical adjustments can reduce risk without relying solely on PPE.
I also appreciate that you highlighted administrative controls, such as following agency policies and IPAC training. These often go unnoticed but play a critical role in keeping both clients and healthcare workers safe. Finally, your reflection about PPE being the last line of defence really reinforces the hierarchy principle: the higher-level controls are more effective in reducing risk.
-
-
2026-01-28 at 6:07 pm #18372MujidatMember
Elimination – Completely removing the hazard. In a hospital setting where I did my placement, a nursing unit used to store cleaning chemicals in patient care areas, posing a risk of accidental exposure. Management relocated all chemicals to a locked, dedicated storage room away from patient areas, effectively eliminating the hazard from the patient care environment.
Substitution – Replacing the hazard with something safer. At a care home, staff were using a strong chemical disinfectant for cleaning that caused respiratory irritation. The facility substituted it with a non-toxic, environmentally friendly disinfectant that provided the same cleaning effectiveness but was safer for staff and residents.
Engineering Controls – Isolating people from the hazard. In a clinical setting, sharps disposal systems (e.g., needle disposal boxes with safety locks) are used to physically isolate the risk of needle-stick injuries from staff handling injections.
Administrative Controls – Changing the way people work. In a long-term care facility, staff schedules were adjusted to reduce fatigue and the risk of lifting injuries. Policies were also implemented to require team lifting for residents over a certain weight. This is an administrative control because it modifies staff behavior and workflow to reduce hazards.
Personal Protective Equipment (PPE) – Protecting the worker when exposure cannot be eliminated.
In a COVID-19 unit, healthcare workers were required to wear masks, gloves, gowns, and face shields to protect themselves from infectious disease. PPE does not remove the hazard but reduces the risk of injury or illness when other controls are insufficient.-
2026-01-30 at 4:50 pm #18393AdetolaMember
Great write-up! I liked the way you clearly explained each level of the hierarchy of controls and used realistic healthcare examples that make the concepts easy to understand. I especially like how you linked each control to a specific setting, such as long-term care and COVID units, which shows practical application rather than just theory. Your examples clearly demonstrate how hazards can be reduced or managed at different levels, and the explanations are concise and relevant to nursing practice. Overall, this is well-organized, accurate, and directly applicable to real clinical environments.
-
-
2026-01-30 at 5:15 pm #18394AdetolaMember
Elimination: Removal of clutter and unused equipment from hallways to reduce trip and fall hazards.
Substitution: Replacement of harsh chemical cleaners with less irritating, safer disinfectants to reduce respiratory risks for staff and patients.
Engineering controls: Use of ceiling lifts and adjustable hospital beds to reduce the risk of musculoskeletal injuries during patient transfers.
Administrative controls: Enforcing policies such as mandatory two-person lifts for dependent patients and scheduled staff education on safe patient handling.
Personal Protective Equipment (PPE): Widely used are gloves, masks, gowns, and face shields, especially when caring for patients with infectious diseases. These measures helped reduce exposure when hazards could not be completely eliminated.
-
2026-01-31 at 8:00 pm #18406MildredMember
Elimination: Removing broken or unsafe equipment from the unit so staff cannot use it.
Substitution: Replacing harsh chemical cleaners with safer, non-toxic disinfectants.
Engineering Controls: Installing ceiling lifts to reduce manual patient handling and prevent staff injuries.
Administrative Controls: Implementing policies such as hand hygiene protocols, staff training, and safe patient-handling guidelines.
Personal Protective Equipment (PPE): Using gloves, masks, gowns, and face shields when providing patient care.
-
2026-02-03 at 8:35 pm #18442MeboMember
Elimination Implementing a “stay at home when sick” policy for staff to remove the hazard (the pathogen) from the building entirely
Substitution Replacing a harsh, skin-irritating disinfectant with an equally effective but less toxic, non-sensitizing alternative
Engineering Controls Installing high-efficiency particulate air (HEPA) filtration systems or point-of-care sharps disposal containers
Administrative Controls Mandating annual IPAC training and implementing “signage” for droplet/contact precautions on patient doors
PPE Providing and requiring the use of N95 respirators, gloves, gowns, and face shields during high-risk procedures
-
-
AuthorPosts
- You must be logged in to reply to this Discussion Thread.